What You Need to Know About Thiamin
| Share on Facebook | Share on Twitter | Share on Google+ |
Thiamin, which is also spelled thiamine, was the first B vitamin to be discovered. Aptly, it was named vitamin B1. The story of the discovery of thiamin goes back nearly 400 years, and is a great example of how science really works.
In the seventeeth century, Japan was reeling from pressures from their first contacts with the "barbarian" explorers from Holland and Spain. The Emperor had closed all of Japan to Western contact except for trading posts in Hiroshima and Nagasaki, and the Imperial Court sought to strengthen the Japanese Navy to ensure that Europeans could be kept away. As the Japanese navy prepared for long-term voyages, hundreds of sailors were lost to a condition the Japanese came to call "sheep-sheep" disease, or, in Japanese, beriberi.
Beriberi was a horrifying condition. In as little as three hours, fit, young sailors would develop fever, delirium, profound muscle weakness, labored breathing, a thready weak pulse, and death. The speed at which symptoms appeared suggested some kind of poisoning, so the best investigators of the day set out to identify the toxin.
The first person to suggest a way of preventing beriberi, however, was not Japanese. A botanist from Germany visiting the Dutch East India trading post in Hiroshima suggested that the problem had to be spoiled rice. Beriberi appeared at the time the samurai were building the first massive storage sheds for long-term rice storage. Sanitation was unknown, and the dampness of the Japanese climate created moldy rice. Rumphius suggested that the sailors simply eat lentils instead of rice, since lentils were less likely to develop mold.
The Imperial High Command rejected this suggestion as the utterance of a barbarian, and beriberi continued to plague Japanese military planners for another 200 years.
In the late 1800's, another Dutch East India employee, a distinguished microbiologist named Christiaan Eijkman, was assigned the problem of preventing beriberi in the native laborers it hired to do construction on the island of Java. Solving the problem of beriberi, Eijkman promised, would just take a few weeks, and then he would retire to a nice red brick cottage in Holland.
For fourteen years, Dr. Eijkman tried to find the beriberi toxin without success. Then Eijkman learned that the Japanese Navy had finally been able to eliminate beriberi by taking white rice out of the diet of its sailors. This was not a major change, because, unlike other people in Eastern Asia, Japanese typically only eat small servings of rice, about 1/3 of a cup (30 grams) or so, at every meal. When the white rice was banished from the ships, beriberi disappeared. With his superior scientific education, Eijkman was sure he would find the toxin in white rice.
Eijkman fed white rice to the chickens in his yard, and they promptly died of "avian beriberi." Using noxious chemicals to make microscope slides to study their brains, Eijkman then spent several years studying chicken brains to determine the toxin. Unfortunately, the only toxin Eijkman located was the red dye he had been using on his slides. Fumes from his slides made him nearly blind, and he was no nearer to identifying the poison.
For Eijkman, the solution was to study more chickens. He fed chickens white rice. He fed chickens red rice, black rice, and brown rice. He gave them rice and distilled water and he even gave some of his chicken's milk of magnesia just to make sure they weren't really dying of constipation. At one point he was feeding his chicken tapioca pudding and schnapps. But there was no toxin and the Dutch East India Company would not let him retire until he could cure beriberi.
Eventually Eijkman heard that a Dutch navy official named van Leent had eliminated beriberi among Dutch sailors after the mess switched from white rice to brown rice. That was it! There had to be a curative compound in brown rice! So, as Eijkman recorded in his diary (which I read from a copy provided by the Eijkman Museum in The Hague) but was not revealed until after his death, Eijkman distilled a "vital amine" from brown rice and then reported to the Dutch East India Company that he had cured beriberi.
He made the story up. He just wanted to go home. But the story got out and suddenly people all over Europe, starting with a Polish nobleman named Casimir Funk, were using brown rice as a miracle cure. At a scientific congress in Berlin, another scientist even gave a pigeon chloroform, and then "cured" it of beriberi by placing a kernel of brown rice in its beak, the pigeon flying out into the audienc. In 1929, Eijkman was awarded the Nobel Prize. Just before his death in 1930, he had tried to return it. But the story gets stranger from there.
A Japanese scientist eventually, in May of 1945, identified the fungus that makes the toxin that causes beriberi. Thiamin helps prevent beriberi, but a deficiency of thiamin isn't what causes it. Publishing this information in a Japanese-language medical journal in May of 1945 was a sure way to make the discovery hard to find. White rice didn't cause beriberi, and brown rice didn't cure it. Vitamin B1 just helped the body deal with the toxin.
Nonetheless, it turned out that there are dozens of diseases that really are related to a thiamine deficiency. Scientists had discovered something without knowing what it was until about a generation later.
This happens a lot more often in science than anyone would be comfortable admitting. (I also have a story about the Warburg hypothesis.) But here's what a century of testing really tells us:
- Wernicke's encephalopathy is the most common manifestation of thiamin deficiency in the modern world. Unlike beriberi, this disease develops over a period of years, not just a few hours. It can cause double vision, or crossed eyes. People who develop this vitamin deficiency syndrome may develop a wide stance and start walking with short steps, or become unable to walk without assistance at all.
- In Korsakov's psychosis, which follows, there may be apathy, or there may be agitation. Patients may hallucinate or they may use available memories to fill in the gaps of their reasoning processes.
Wernicke-Korsakov syndrome most commonly occurs among alcoholics and people who drink very heavily who are not diagnosed with alcoholism. Chronic alcohol exposure changes the enterocytes lining the intestines so that they cannot absorb thiamin from food.
This syndrome can also occur after gastric bypass surgery, when the stomach or intestine has to be removed to treat cancer, when there is severe morning sickness in early pregnancy, and when there is HIV or AIDS. Severe thiamin deficiency can occur with anorexia, and has been observed in prisoners of war and concentration camp survivors. Almost anyone who displays these symptoms will be hospitalized, and treated with 100 mg of thiamin hydrochloride (thiamin HCl) a day. When the conditions that caused thiamin deficiency are corrected and thiamin levels are brought back to normal-which may take as little as 5 days-drastic improvement is not unusual. Only about 20% of people who have had this kind of thiamin deprivation, however, completely return to normal.
Wernicke-Korsakov syndrome is surprisingly common. Up to 3% of the population of developed countries can have this level of thiamin deficiency. In addition to disease conditions that interfere with the absorption of thiamin or the consumption food, simple malnutrition can also cause the disease. Homeless people and older people who live alone are at greatest risk. For the other 97% of the population, however, taking thiamin is not about correcting deficiency. It is about supporting recovery from diseases that have causes other than nutritional deficiency.
Medications That Cause Depletion of Thiamin
The most common cause of B-vitamin deficiency in elderly adults in the United States is the use of the diuretic Lasix (furosemide), which causes the tubes of the kidneys to send thiamin and other B vitamins, as well as magnesium and potassium, into the urine. Thiamin deficiency also occurs in people who are on dialysis.
Anti-Thiamin Factors in Food
Certain foods contain anti-thiamin factors that oxidize the vitamin to form an inert product. Foods that can cause thiamin depletion include:
- Excessive amounts of coffee and tea, including decaffeinated coffee and tea,
- Silkworms, a common food in Nigeria (where a condition called seasonal ataxia occurs during the time of year silkworms are most commonly eaten),
- Certain raw fish and shellfish, such as alewife, herring (eaten pickled), shad, and trout,
- Fiddlehead ferns, and
- Foods made with sulfites, such as sausage, lager beer, white wine, and fast food burgers.
Thiamin deficiency resulting from massive consumption of these foods is rare but not unknown.
Foods That Are Rich In Thiamin

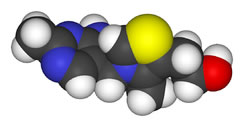
On the other hand, certain foods are excellent sources of thiamin. Thiamin occurs in food as free thiamin, and also as certainly chemically modified forms of phosphate: thiamin monophosphate (TMP), thiamin triphosphate (TTP), and thiamin pyrophosphate (TPP), which is also known as thiamin diphosphate.
| Food | Serving | Thiamin (mg) |
| Brazil nuts | 1 ounce (28 grams) | 0.18 |
| Cantaloupe | 1/2 fruit (150 grams) | 0.11 |
| Egg (cooked) | 1 large | 0.03 |
| Fortified breakfast cereal | 1 cup (80 grams) | 0.5-2.0 |
| Lentils (cooked) | 1/2 cup (35 grams) | 0.17 |
| Long grain brown rice (cooked) | 1 cup (80 grams) | 0.19 |
| Long grain white rice, enriched (cooked) | 1 cup (80 grams) | 0.26 |
| Long grain white rice, unenriched (cooked) | 1 cup (80 grams) | 0.04 |
| Milk | 1 cup (240 ml) | 0.10 |
| Orange | 1 fruit | 0.10 |
| Peas (cooked) | 1/2 cup (40 grams) | 0.21 |
| Pecans | 1 ounce (28 grams) | 0.19 |
| Pork, lean (cooked) | 3 ounces (84 grams) | 0.72 |
| Spinach (cooked) | 1/2 cup (22 grams) | 0.09 |
| Wheat germ breakfast cereal | 1 cup (115 grams) | 4.47 |
| White bread, enriched | 1 slice | 0.11 |
| Whole wheat bread | 1 slice | 0.10 |
Fortified cereals, wheat germ, and pork are particularly thiamin-rich foods. The thiamin content of most foods is reduced during cooking. (Loss during cooking has been taken into account in the table above.)
How Much Thiamin Do You Need to Prevent Deficiency?
It's not hard to prevent thiamin deficiency. Here are the Recommended Dietary Intakes determined by the US Food and Nutrition Board in 1998:
| Life Stage | Age | Males (mg/day) | Females (mg/day) |
| Infants | 0-6 months | 0.2 | 0.2 |
| Infants | 7-12 months | 0.3 | 0.3 |
| Children | 1-3 years | 0.5 | 0.5 |
| Children | 4-8 years | 0.6 | 0.6 |
| Children | 9-13 years | 0.9 | 0.9 |
| Adolescents | 14-18 years | 1.2 | 1.0 |
| Adults | 19 years and up | 1.2 | 1.1 |
| Pregnant Women | Any age | - | 1.4 |
| Breastfeeding Mothers | Any age | - | 1.4 |
There is no upper limit for thiamin supplementation. Even when it is taken in doses greater than 200 milligrams a day, adverse effects have not been observed, although theoretically an intravenous dosage of thiamin would be more likely to provoke an adverse reaction.
These amounts of thiamin, however, are only the recommendation for the prevention of deficiency. Much larger amounts of thiamin are used to support recovery from disease.
Thiamin for Alzheimer's Disease
Bloodstream levels of thiamin and related enzymes are usually lower in people who have Alzheimer's disease. Various dosages of thiamin have been tested to see if they help symptoms.
- A preliminary study found that dosages of 3,000 to 8,000 mg of thiamin per day had small benefits in Alzheimer's patients, but the follow-up study was never conducted.
- A clinical trial found no benefit in giving Alzheimer's patients 3,000 mg per day for a year.
- A third clinical study found thiamin benefits in Alzheimer's disease in patients given 100 mg a day of a thiamin derivative called thiamin tetrahydrofurfuryl disulfide.
Frankly, I only recommend giving people with Alzheimer's disease enough thiamin to prevent thiamin deficiency at this time. It is difficult to get people with Alzheimer's to take pills, and both patient and caregiver need to minimize stress.
Thiamin and Cancer
Several doctors in Germany and Poland successfully treat cancer by restricting thiamin. Thiamin is essential for the formation of a class of enzymes called the transketolases. These enzymes are make it possible for the cell to make DNA prior to cell division. If you have cancer of any kind, don't take thiamin supplements unless you have a medically diagnosed thiamin deficiency.
Thiamin and Congestive Heart Failure
Almost all congestive heart failure patients are put on diuretics to lower blood volume and to reduce the stress on the heart. One study found that 98% of patients given 80 mg of furosemide (Lasix) per day or more developed thiamin deficiencies, and that that thiamin supplements restored the function of the left ventricle-relieving congestive heart failure.
I myself have seen remarkable improvement in congestive heart failure patients who just start taking a complete B-vitamin supplement offering 100 to 1000% of the RDI of thiamin. If you don't also have active cancer, taking supplemental thiamin may be a great way to reduce the side effects of treatment with diuretics.
Frequently Asked Questions About Thiamin
Q. Are there any thiamin deficiency symptoms that are a signal I need to take supplemental thiamin?
A. If you:
- Take medication for seizures, or
- Take diuretics for congestive heart failure, or
- Drink alcohol heavily, or
- Have an eating disorder such as anorexia, or
- Have had gastric bypass or similar surgery, and
- You do NOT have cancer, then
You should be on the lookout for:
- Irritability,
- Mood swings,
- Memory loss,
- Burning sensations in the toes and feet and then in the legs and hands,
- Loss of appetite,
- "Sluggish" digestion,
- Muscle tremors, and
- Shortness of breath, and that order.
Symptoms of thiamin deficiency typically "kick in" about two weeks after the vitamin is withdrawn from the diet. All the symptoms do not occur at once. Symptoms often can be treated in just a few days, if they have not be neglected so long that nerve damage occurs.
Q. Should I take a thiamin mononitrate supplement?
A. No, thiamin mononitrate is an especially heat-stable form of thiamin added to flour before it is baked into bread.
Q. Should I get a thiamin injection for thiamin deficiency?
A. If you have a medically diagnosed thiamin deficiency, your doctor will probably offer a thiamin injection. Injection is usually reserved for treatment of severe symptoms.
Q. What of thiamin is thiamin MSDS?
A. An MSDS is a Material Safety Data Sheet that tells manufacturers what to do in case of chemical spills on the factory floor.
Q. Is there a potentially toxic level of thiamin overdose?
A. Scientists know from safety testing using laboratory mice that if you were to take about 8% of your body weight in thiamin, that is, up to 10 or 20 pounds (5-10 kilos) of thiamin powder, you would experience various toxic effects. You can't do this because there is no way for your digestive tract to absorb that much thiamin.
Q. Do dogs and cats need thiamin, too?
A. Yes, thiamin is essential for all kinds of animals, although thiamin deficiency is rare except in birds.
Selected References:
Bender DA. Optimum nutrition: thiamin, biotin and pantothenate. Proc Nutr Soc. 1999;58(2):427-433.
Boros LG, Brandes JL, Lee WN, et al. Thiamine supplementation to cancer patients: a double edged sword. Anticancer Res. 1998;18(1B):595-602.
Brody T. Nutritional Biochemistry. 2nd ed. San Diego: Academic Press; 1999.
Comin-Anduix B, Boren J, Martinez S, et al. The effect of thiamine supplementation on tumour proliferation. A metabolic control analysis study. Eur J Biochem. 2001;268(15):4177-4182.
Cumming RG, Mitchell P, Smith W. Diet and cataract: the Blue Mountains Eye Study. Ophthalmology. 2000;107(3):450-456.
Flodin N. Pharmacology of micronutrients. New York: Alan R. Liss, Inc.; 1988.
Food and Nutrition Board, Institute of Medicine. Thiamin. Dietary Reference Intakes: Thiamin, Riboflavin, Niacin, Vitamin B6, Vitamin B12, Pantothenic Acid, Biotin, and Choline. Washington D.C.: National Academy Press; 1998:58-86.
Glaso M, Nordbo G, Diep L, Bohmer T. Reduced concentrations of several vitamins in normal weight patients with late-onset dementia of the Alzheimer type without vascular disease. J Nutr Health Aging. 2004;8(5):407-413.
Hendler SS, Rorvik DR, eds. PDR for Nutritional Supplements. Montvale: Medical Economics Company, Inc; 2001.
Heroux M, Raghavendra Rao VL, Lavoie J, Richardson JS, Butterworth RF. Alterations of thiamine phosphorylation and of thiamine-dependent enzymes in Alzheimer's disease. Metab Brain Dis. 1996;11(1):81-88.
Hung SC, Hung SH, Tarng DC, Yang WC, Chen TW, Huang TP. Thiamine deficiency and unexplained encephalopathy in hemodialysis and peritoneal dialysis patients. Am J Kidney Dis. 2001;38(5):941-947.
Jacques PF, Taylor A, Moeller S, et al. Long-term nutrient intake and 5-year change in nuclear lens opacities. Arch Ophthalmol. 2005;123(4):517-526.
Kish SJ. Brain energy metabolizing enzymes in Alzheimer's disease: alpha-ketoglutarate dehydrogenase complex and cytochrome oxidase. Ann N Y Acad Sci. 1997;826:218-228.
Krishna S, Taylor AM, Supanaranond W, et al. Thiamine deficiency and malaria in adults from southeast Asia. Lancet. 1999;353(9152):546-549.
Leslie D, Gheorghiade M. Is there a role for thiamine supplementation in the management of heart failure? Am Heart J. 1996;131(6):1248-1250.
Mastrogiacoma F, Bettendorff L, Grisar T, Kish SJ. Brain thiamine, its phosphate esters, and its metabolizing enzymes in Alzheimer's disease. Ann Neurol. 1996;39(5):585-591.
Meador K, Loring D, Nichols M, et al. Preliminary findings of high-dose thiamine in dementia of Alzheimer's type. J Geriatr Psychiatry Neurol. 1993;6(4):222-229.
Mimori Y, Katsuoka H, Nakamura S. Thiamine therapy in Alzheimer's disease. Metab Brain Dis. 1996;11(1):89-94.
Muri RM, Von Overbeck J, Furrer J, Ballmer PE. Thiamin deficiency in HIV-positive patients: evaluation by erythrocyte transketolase activity and thiamin pyrophosphate effect. Clin Nutr. 1999;18(6):375-378.
Nishimune T, Watanabe Y, Okazaki H, Akai H. Thiamin is decomposed due to Anaphe spp. entomophagy in seasonal ataxia patients in Nigeria. J Nutr. 2000;130(6):1625-1628.
Rieck J, Halkin H, Almog S, et al. Urinary loss of thiamine is increased by low doses of furosemide in healthy volunteers. J Lab Clin Med. 1999;134(3):238-243.
Rindi G. Thiamin. In: Ziegler EE, Filer LJ, eds. Present Knowledge in Nutrition. 7th ed. Washington D.C.: ILSI Press; 1996:160-166.
Rodriguez-Martin JL, Qizilbash N, Lopez-Arrieta JM. Thiamine for Alzheimer's disease (Cochrane Review). Cochrane Database Syst Rev. 2001;2:CD001498.
Russell RM, Suter PM. Vitamin requirements of elderly people: an update. Am J Clin Nutr. 1993;58(1):4-14.
Schumann K. Interactions between drugs and vitamins at advanced age. Int J Vitam Nutr Res. 1999;69(3):173-178.
Shimon I, Almog S, Vered Z, et al. Improved left ventricular function after thiamine supplementation in patients with congestive heart failure receiving long-term furosemide therapy. Am J Med. 1995;98(5):485-490.
Suter PM, Haller J, Hany A, Vetter W. Diuretic use: a risk for subclinical thiamine deficiency in elderly patients. J Nutr Health Aging. 2000;4(2):69-71.
Tanphaichitr V. Thiamin. In: Shils M, Olson JA, Shike M, Ross AC, eds. Modern Nutrition in Health and Disease. 9th ed. Baltimore: Williams & Wilkins; 1999:381-389.
Todd K, Butterworth RF. Mechanisms of selective neuronal cell death due to thiamine deficiency. Ann N Y Acad Sci. 1999;893:404-411.
Wilcox CS. Do diuretics cause thiamine deficiency? J Lab Clin Med. 1999;134(3):192-193.
Wilkinson TJ, Hanger HC, George PM, Sainsbury R. Is thiamine deficiency in elderly people related to age or co-morbidity? Age Ageing. 2000;29(2):111-116.
Zenuk C, Healey J, Donnelly J, Vaillancourt R, Almalki Y, Smith S. Thiamine deficiency in congestive heart failure patients receiving long term furosemide therapy. Can J Clin Pharmacol. 2003;10(4):184-188.
-
Skin CareMen Skin Care
-
Free ResourcesFree eBooks
-
Whatever we put our attention on will grow stronger in our life.Maharishi Mahesh Yogi
-
What We RecommendIf you do an analysis of the ingredients in a bottle of
 Total Balance and compare with other products you will find that it provides exceptional value for money…even against simple mass produced products with lower bottle costs.
Total Balance and compare with other products you will find that it provides exceptional value for money…even against simple mass produced products with lower bottle costs.
-